 12 Aug 2019
12 Aug 2019
If you’re worried you might have gum disease, there’s good reason for that. Gum disease affects nearly half of the U.S. adult population. That’s just under 65 million people! It’s one of the most common reasons people see the dentist.
So, are you at risk?
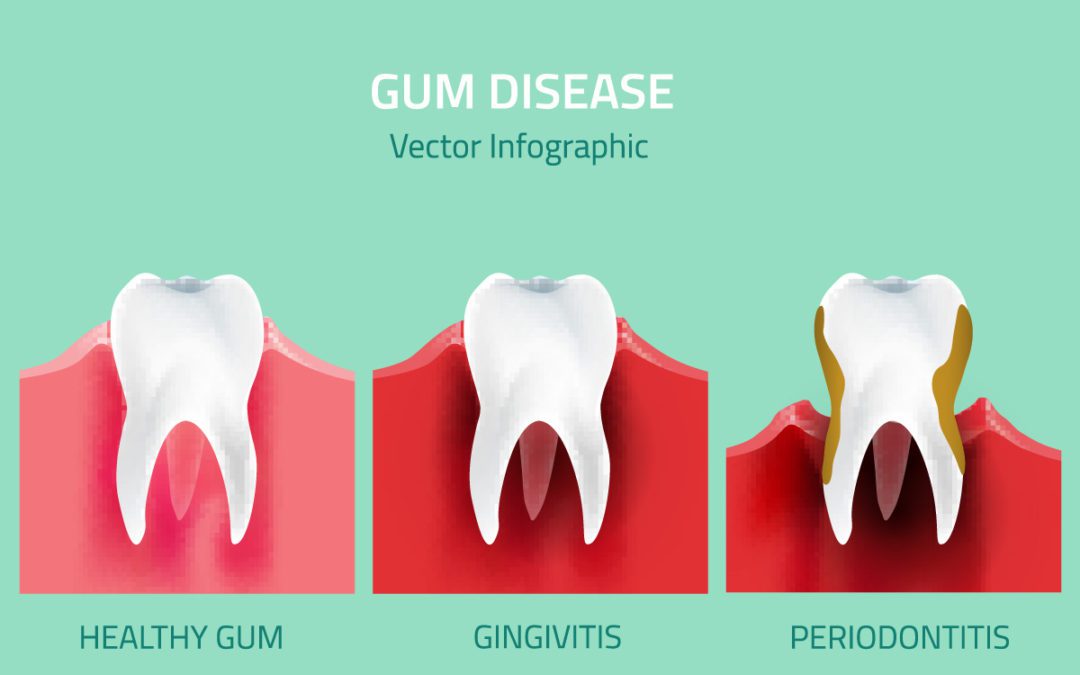
Gum disease (known as periodontal disease) has serious consequences for your dental health. It’s a chronic condition that can proceed quickly in different people. In the worst cases, it results in teeth that are infected and loose and need to be removed.
We know that bleeding gums is closely connected to how we brush and floss. And most people don’t brush and floss enough. But removing plaque is one part of the story. Gum disease is a sign of many other problems throughout the body. If you suspect you have gum disease, then these four signs may tell you it’s time to see the dentist.
1) Bleeding Gums
Gums should not bleed when you brush and floss. As a general rule, if you aren’t a routine flosser, bacteria buildup below the gums may cause your gums to bleed each time you brush. This can also spread and cause bleeding when you brush your gums. If the problem persists, the bleeding usually worsens.
Gum swelling, red gums, or sore gums may also accompany bleeding. Tooth sensitivity may occur as well and may be due to gum recession from the infected, bleeding gums. It’s common to ask if you should stop flossing when your gums are bleeding.
If you don’t floss, the plaque that causes gingivitis will destroy the fibers that attach your gum tissue to your teeth. This plaque has bacteria that cause the inflammation in your gums.
With gums that bleed, there is much more to consider than just the pain or discomfort associated with the bleeding itself. Even though that is enough for most people to be concerned with, there are more problems that can take place after bleeding has begun if it is related to gum disease.
When your blood is delivering immune cells to exit your tissue, it makes sense that this may make way for other things to enter the bloodstream. If this is the case, harmful bacteria that are formed in the mouth can gain access to your bloodstream and cause a number of problems.
These bacteria bond to platelets in the blood and cause clots, which can lead to heart attack or stroke. If this happens, then a whole host of potential health effects can occur. Gum disease has some serious conditions associated with it. There are strong links with heart attack and stroke. When you see bleeding gums it’s time to get your dental checkup.
Your dentist will perform an exam that is designed to measure the severity of your bleeding gums. There are some general stages of bleeding gums that you can be aware of:
- Bleeding after or during brushing: This is when you will spot red or dark spots on your brush or floss. Your goal here is to disturb plaque, so it shows you’re doing the right thing.
- Gums begin to bleed more frequently: Instead of bleeding just on brushing, you’re now finding blood when you eat or without any stimulation at all.
- Bleeding happens on its own, not just when brushing: Sometimes, gums will bleed with no stimulus at all. This is a sign that inflammation is progressing to more serious stages.
- Gums begin to darken from light pink to a deeper red: This shows that more immune-regulated cells are located in the vessels. Gingivitis progresses as the immune response worsens. It signals processes that eat away at the gum tissue. Light, red blood is a sign there is oxygen present. Darker gums show lack of oxygen which is related to types of bacteria that thrive in an oxygen-free environment.
2) Gum Recession or Gum Pocketing
Do your teeth look like they are getting longer? Teeth that appear “long” may be due to fact that the gums that surround them are receding away. Gum recession is a sign that gum disease is progressing.
When this happens, the depth of the collar of gum tissue around your teeth increases. In later stage gum disease, these pockets become too deep. The problem is that it then becomes difficult to remove the food and debris by brushing and flossing. This causes the pockets to become progressively deeper and the gum disease to worsen.
Unfortunately, to most, gum recession is considered to be a normal part of aging. You may have heard the expression “long in the tooth” to describe getting older. This refers to how the gum line tends to recede and expose more of the surface of our teeth.
There really is nothing normal or inevitable about gum recession. For most of us, it can be prevented.
Gum recession and pockets are not the same:
- Gum recession is the loss of gum tissue from around the tooth, exposing the root. Measurements are taken along the outer surface of the tooth to gauge how much gum has recessed or migrated over time. Measurements vary per person in the sense that a 4mm reading might be fine in one person but may not be for another. By taking a measurement and keeping track of its progression, we are able to determine different recommendations for taking care of your teeth and get a specialist involved if needed.
- Gum pockets are the space between the gums and teeth. Dentists measure gum pockets by “probing” or “charting” to determine the general periodontal or gum health. A probe is placed down in between the tooth and the gums to determine where the attachment of gum starts. This is known as the bottom of the pocket. Hygienists and dentists take six measurements for every tooth to evaluate the health or presence of gum disease. By keeping a record of this year after year we hope to maintain a healthy periodontium and prevent periodontal disease and tooth loss. A normal or healthy range is between 1mm and 3mm, anything higher is indicative of infection and gum disease.
3) Tooth Sensitivity
Gum recession or pocketing can lead to tooth sensitivity. In these cases, sensitivity can be a sign of gum disease. Chronically inflamed gum tissue is exposing the root surface of the tooth. This exposed root makes the tooth more susceptible to decay, abfraction (wear in the root surface), tooth sensitivity, and potential tooth loss.
Tooth sensitivity occurs when consuming things like cold or hot beverages. If your symptoms are worsening, it’s time to see your dentist to see if they may be related to gum disease.
4) High Blood Sugar
If your blood sugar is high, you may have or be at risk of type 2 diabetes. The link between gum disease and type 2 diabetes is two-directional. People with type 2 diabetes have a higher risk of gum disease that progresses faster. That’s why it’s important for your dentist to know whether you have type 2 diabetes or not.
Signs of high blood sugar include:
- Increased thirst
- Headaches
- Mind fog or trouble concentrating
- Blurred or impaired vision
- Frequent urination
- Fatigue or loss of energy (weak, tired feeling)
- Unexplained weight loss
If you experience any of these conditions, you should see your general practitioner to test your blood sugar.
However, if you see your dentist and have been diagnosed with gum disease, you should also test your blood sugar. The conditions are closely connected to general inflammation in the body.
General Steps to Controlling Your Gum Disease
Visit your dentist for a professional dental exam and cleaning. In order for gum disease to settle, you will need to brush and floss.
Try to tie flossing and brushing to meal times or a time that is convenient for your schedule. Floss, then brush your teeth and tongue: (1) when you first wake up, (2) when you first return home from school or work (don’t come out of the bathroom until you do), and (3) before bed.
Once your oral hygiene is in order, you can assess if the signs of gum disease are improving or not. The objective is to disturb the plaque and bacteria preventing it from sitting too long.
If you do this, advanced calculus (tartar) will never be able to attach to your teeth. Many people say that they think twice a day is enough. Well, what happens if you miss one of those two times? The plaque living in bacteria will then begin to start to grow on the tooth surface in the next eight hours.
OK, if you brush at night, why do you still have to brush in the morning? This is why you should. You are cleaning, not sterilizing your mouth. There are still living organisms in there. Your body is working while you are sleeping, digesting food, growing fingernails, etc. Bacteria performs many processes and plaque forms.
It’s not hard to imagine why your gums become infected and bleed now, is it (especially if you do this day in and day out)? But remember that your oral hygiene is one part of gum disease. Bleeding gums and inflammation that occurs in the mouth likely happens elsewhere in the body as well.
Gum disease can be a sign of the general health of your body. See it as a dashboard for other issues in your mouth, gut, immune system, and heart.
